The International Headache Society devised a classification for migraine headaches in 1988 which distinguishes between headaches with aura (vision affected) and those without aura.

Migraine headaches are intermittent and may vary in frequency from year to year, and therefore are difficult to measure.
The causes of migraines are unknown, but there may be a disturbance of intracranial and extracranial circulation. The disturbance in blood flow is believed to accompany the migraine attack and possibly cause it.
“A migraine is like a tornado; it attacks fast without any warning and wreaks havoc. ”
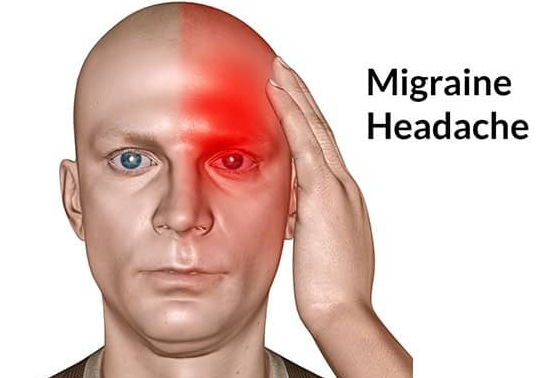
Migraines usually start during the teenage years or early in adult life, affecting more women than men with a ratio of three to one. Migraines are caused from constricted (tightening) arteries that supply blood flow to the brain. When the arteries constrict, blood flow to the brain is reduced as well as the brains oxygen supply. The brain reacts by dilating (enlarging) arteries to meet the brain’s need for energy. The dilation spreads to the arteries in the neck and scalp and is the culprit of the pain in migraines.
If you live with migraines, make sure to have your Doctor rule out an underlying illness or other medical conditions that mimic migraines with the appropriate tests: for example , x-rays determining sinus infection, EEG for seizure activity or a CAT scan to detect blood clots or a brain tumor. Your Dr . may determine a drug to help ease your pain.
Eight Migraine Triggers
1 . Cerviogentic Headache:
Some people who have a tender neck and suffer from sore bone and joint problems are diagnosed with this type
2 . Temporomandibular Migraine:
Triggered by teeth grinding
3. Sinus Migraine:
Triggered by allergies and caused by excessive mucous and often accompanied by a fever. If you have this type of migraine, you may experience pain around both eyes and also may feel nauseated and sensitive to light.
4. Genetic Migraines:
Studies have lined a gene to people affected with migraines. Often when the gene for migraines is passed on to the next generation, the recipient will also experience headaches around the same age as the person who passed on the migraine.
5. Stress Migraine:
Stress can be a major contributing factor to the onset of a migraine. Type A personalities are more likely to experience migraines. Type A is ambitious, bright, perfectionist, emotionally repressed, cautious and has a decreased ability to manage stress. However , this is the easiest type of migraine to treat because a type A personality can acquire the skills necessary to manage stress.
6. Hormonal Migraine:
Fluctuating hormones in women are often the cause of migraines and can happen during menstrual cycles.
7. Cigarette Migraine
An equal opportunity source of migraines is because the nicotine alters blood vessels. High carbon monoxide levels in a person who smokes or even inhales second hand smoke can lead to a migraine.
8. Food Migraines
Food allergies are another factor that leads to migraines. However , migraine sufferers are able to eat chocolate without falling prey to a migraine. Some patients actually report relief from eating chocolate.
Foods that Can Cause Migraines
1 . Aged cheese such as Roquefort, Stilton and Sharp Cheddar
2 . Fermented Dairy such as Sour Cream, Buttermilk and Yogurt
3. Citrus: Oranges or Grapefruit, including juice
4. Nuts: Peanuts, Walnuts or Pecans
5. Legumes: Peas, Beans and Soy product 6. Onions and Garlic
7. Bananas
8. Pickled or Salty foods: picked herring is the most common instigator
9. MSG found in Chinese food
10. Alcohol
11. Artificial sweeteners
12. Caffeine (getting too much or withdrawal)
13. Chocolate
14. Cured meats
15. Dried fish
16. Dried fruits
17. Food additives (nitrites, nitrates, MSG)
18. Lunch meats (cured with nitrites or MSG)
19. Odors
20. Onions
21. Skipped meals
Now that you know the common triggers, also note that skipping meals also causes migraines. Skipping meals causes your blood sugar to drop, which in turn causes a migraine.
Other Migraine Triggers
1. Dehydration
2. Depression
3. Exercise (too much)
4. Eyestrain or other visual triggers
5. Fatigue (extreme)
6. Lights (bright or flickering; sunlight, particularly glare)
7. Menstrual periods
8.Medications
9. Noise (too much)
10. Odors
11. Sleep (too much, too little, other changes)
12. Stress
13. Watching TV or movies
14. Weather (changing conditions)
Six Ways to Kiss Your Migraine Goodbye
1. Natural products
Magnesium supplements (600 mg) decreased migraine attacks. Fish oils may decrease migraine attacks through their effects.
USANA Essentials and Coquinone 30 are your sure way to kick migraine !
USANA Essentials is rich with Riboflavin, the water-soluble vitamin B2, improves energy metabolism in the body, as does coenzyme Q10 in Coquinone!
Riboflavin is sometimes used as a migraine preventative treatment (prophylaxis).
It is further thought that taking a riboflavin supplement has the potential to increase the mitochondrial energy efficiency in an individual who has migraine.
In short riboflavin would be taken with the aim of improving the way oxygen is metabolized (Distribution) in the brain improving Migraine conditions!
2. OTC and Prescriptoin Medicine
Medicines have been used for centuries to treat migraines. Today Dr’s prescribe Beta Blockers to treat migraines by maintaining adequate dilation of blood vessels. Antidepressants: The brain chemical ‘serotonin’ plays a role in migraine attacks because the levels of serotonin may cause or relieve migraine and that’s why Drs sometimes prescribe antidepressants for migraines. Antidepressants reduce migraine frequency by regulating serotonin levels in the brain. Other drugs are triptans available as an injection or nasal spray. This type of drug shuts down the inflammation and transmission of migraine pain.
Fioricet contains a combination of acetaminophen, butalbital, and caffeine Acetaminophen is a pain reliever and fever reducer. Butalbital is in a group of drugs called barbiturates. It relaxes muscle contractions involved in a tension headache. Caffeine is a central nervous system stimulant. It relaxes muscle contractions in blood vessels to improve blood flow.
Fioricet is used to treat tension headaches that are caused by muscle contractions.
Gabapentin is a very good prescription for migraine prevention
3 . Surgical Treatment
Nerve stimulators have been used to control back and muscle pain and in 2003 a nerve stimulator was successfully used to treat chronic headaches. With nerve stimulation, one end of a wire is connected to a nerve that controls pain and the other is connected to a small battery powered generator. The patient controls the generator via a remote device. Once turned on, it disconnects the pain signal.
Not only do chronic migraine suffers face agonizing physical disabilities, they also have the psychological fear of not being able to earn a living or manage their home life because daily activities can suddenly become unbearable with the onset of a migraine.
4. Holistic Intervention
Rarely are people offered a non drug approach to treating migraines. Treating a migraine holistically not only can treat the migraine at onset but can also act as prevention.
Create a headache diary listing the 5 W’s.
A. Who were you with?
B. Where? Did someone irritate you? At work with glaring lights?
C. What? What medications were you on?
D. When? When did the headache start?
E. Why? Did some particular food or drink aggravate the situation? Did you get enough sleep?
5. Review your diary after 30 days and see if you can isolate the trigger.
6. Use heat to help dilate the blood vessels in the body.
This must be done at direct onset of your migraine. Soak your hands in hot water for 20-30 minutes. As the migraine progresses and the blood vessels enlarge, apply ice to the back of the neck and forehead to help constrict capillaries that are pressing against the nerves.
7. Relaxation techniques
You can use relaxation techniques to manage stress. Research has found that people who consciously practice yoga daily for 30 – 45 minutes can learn to positively manipulate involuntary bodily responses like migraine pain. Studies have shown that relaxation practiced on a regular basis achieves a 45 to 80% reduction or elimination in both migraine severity and frequency. Yoga triggers a boost in the brain chemical serotonin, a neurotransmitter that is involved with your body’s anger, pain, sleep and migraine and can be a cure for headaches.
Frequent headaches are a sign that you are stressed out and it’s your body’s way of saying slow down and take care of me. Especially if you are a type A personality. My type A patients often say they can’t sit still and have a difficult time with the relaxation/mediation part of yoga. My reply? What’s more difficult to live with. Meditating daily or living with a migraine, a stroke or a heart attack? These are very real situations that afflict people with constricted arteries and that’s why it’s vital that you make time for your health.
Unfortunately for my patients, I often meet them after they’ve suffered from a condition of vascular abnormality. They are very motivated to participate because they have experienced what happens when blood flow to the heart or brain is compromised. Consequently they practice my techniques daily to reduce a recurrence.
Why not make time now? There are 1440 minutes in a day. 45 minutes a day practicing yoga is a wise investment in your health that offers a positive life style with increased energy without the use of toxic drugs polluting your liver and fewer Doctor visits which equals fewer co-payments. Yoga Chi for Energy DVD includes medically engineered relaxation techniques with an 11 minute meditation by a crackling fireplace.
