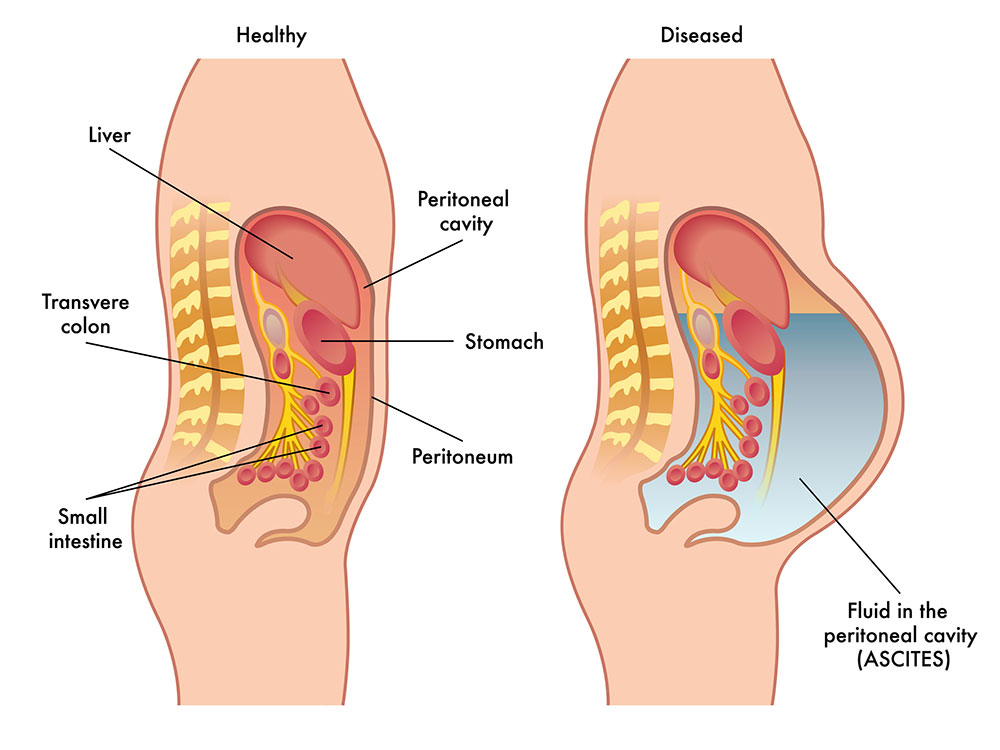
Ascites is a condition in which fluid collects in spaces within your abdomen. If severe, ascites may be painful. The problem may keep you from moving around comfortably. Ascites can set the stage for an infection in your abdomen. Fluid may also move into your chest and surround your lungs. This makes it hard to breathe. Ascites is diagnosed based on physical exam, medical history, blood tests, ultrasound or CT scan, and paracentesis. Paracentesis is a procedure in which a needle is inserted through the abdominal wall (after local anesthesia) and fluid is removed. This fluid is examined for signs of infection, cancer, or other medical problems.
What causes ascites?
The most common cause of ascites is cirrhosis of the liver. Drinking too much alcohol is one of the most common causes of cirrhosis of the liver.
Different types of cancer can also cause this condition. Ascites caused by cancer most often occur with advanced or recurrent cancer. Ascites may also be caused by other problems such as heart conditions, dialysis, low protein levels, and infection.
What are the symptoms of ascites?
These are symptoms of ascites:
- Swelling in the abdomen
- Weight gain
- Sense of fullness
- Bloating
- Sense of heaviness
- Nausea or indigestion
- Vomiting
- Swelling in the lower legs
- Shortness of breath
- Hemorrhoids
What are the complications of ascites?
- Abdominal pain, discomfort and difficulty breathing: These problems may occur when too much fluid builds up in the abdominal cavity. This may limit a patient’s ability to eat, walk and perform daily activities.
- Infection: The fluids that build up in the gut as a result of ascites could become infected with bacteria. When this happens, the condition is called spontaneous bacterial peritonitis. It usually causes fever and abdominal pain. The diagnosis is generally made by taking a sample from the abdominal cavity as described above (ie, by performing a paracentesis). Spontaneous bacterial peritonitis is a serious condition that requires treatment with IV antibiotics. After recovery from this infection, long-term treatment with oral antibiotics is needed to keep the infection from recurring.
- Fluid in the lungs: This condition is called hepatic hydrothorax. Abdominal fluid fills the lung (mostly on the right side). This results in shortness of breath, cough, hypoxemia (lack of oxygen in the blood) and/or chest discomfort. Hepatic hydrothorax is best treated by removing the abdominal ascites by paracentesis.
- Kidney failure: Worsening of cirrhosis of the liver can lead to kidney failure. This condition is called hepatorenal syndrome. It is rare, but is a serious condition and may lead to kidney failure.
How is ascites diagnosed?
Your healthcare provider will do a physical exam and ask about your symptoms. You may also have tests such as:
- Fluid sample. A sample of fluid from your abdomen may be taken using a needle. This fluid will be checked for signs of disease, such as cancer or an infection. This test may help point to the cause of the ascites.
- Imaging. Your healthcare provider may request images of the inside of your abdomen using ultrasound, MRI, or a CT scan. An MRI creates images using a magnetic field and radiofrequency energy. A CT scan creates computerized images using X-rays.
How is ascites treated?
A number of steps may help ease your ascites. Your healthcare provider may tell you to:
- Cut back on your salt intake. Your healthcare provider or a dietitian can show you how to follow a low-sodium diet. Avoid salt substitutes that contain potassium. This is because some medicines used in treating ascites can cause your potassium levels to rise.
- Cut back on the amount of fluids you drink.
- Stop drinking alcohol.
- Take diuretic medicines to help reduce the fluid in your body.
- In certain cases, your doctor may need to remove large amounts of fluid from your abdomen through a needle. This may be done if you have trouble breathing or the diuretic is not working.
- In very complicated situations, you may need to have a special procedure in radiology called TIPS. In this procedure, a connection is made inside the liver between the blood vessels to ease the high pressure causing ascites.
What are the best treatments for ascites?
Limit the amount of salt in your diet. The most important step to treating ascites is to drastically reduce your salt intake. Recommended limits are 2,000 mg or less a day. Seeing a nutritional specialist (dietitian) is helpful especially because the salt content in foods is difficult to determine. Salt substitutes — that do not contain potassium — can be used.
Often, patients will require diuretics (“water pills”) to treat ascites. Take these pills as prescribed. Common diuretics are spironolactone (Aldactone®) and/or furosemide (Lasix®). These water pills can cause problems with your electrolytes (sodium, potassium) and kidney function (creatinine). Taking water pills is not a substitute for reducing your salt intake. Both are needed to treat ascites.
Other, increasingly more aggressive treatments include:
- Paracentesis as a treatment: Sometimes fluids continue to build up in the abdomen despite use of diuretics and a restricted salt diet. In these cases, patients may need paracentesis to remove this large amount of excess fluid.
- Surgery: Surgical placement of a shunt (tube) between the main vein (portal vein) and smaller veins is sometimes used as a treatment. A radiologist can place a shunt directly through the liver, thereby relieving portal hypertension and diminishing ascites. By increasing blood flow, all organs of the body are better able to perform their function. For example, in patients with ascites, improved kidney function helps rid the body of excess sodium (salt) and prevent the buildup of fluids.
- Liver transplant:** **This approach is reserved for patients with very severe cirrhosis whose livers are failing.
Can ascites be prevented?
Certain steps to help you avoid cirrhosis of the liver and cancer can prevent ascites. These include:
- Stop drinking alcohol.
- Maintain a healthy weight.
- Exercise regularly.
- Stop smoking.
- Limit salt in your diet.
- Practice safe sex to decrease your chance of getting hepatitis.
- Do not use recreational drugs to decrease your chance of getting hepatitis.
What can I do to control my ascites?
- Weigh yourself daily. Call your doctor if you gain more than 10 lbs (or more than 2 lbs per day on 3 consecutive days).
- Limit the amount of alcohol you drink. Better yet, do not drink any alcoholic beverages at all. Reducing the amount of alcohol you drink reduces the risk of developing ascites.
- Limit use of nonsteroidal anti-inflammatory drugs (NSAIDs). Ibuprofen (Advil®, Motrin®), aspirin, indomethacin, sulindac are examples of NSAIDs. These drugs affect the kidneys, causing water and salt to be retained by the body.
- Follow guidelines for a low-salt diet. Recommended limits are 2,000 mg or less a day.
Living with ascites
Be sure to follow your healthcare provider’s advice for lowering your salt intake. You’ll need to do this even if you’re taking diuretic drugs to reduce fluid in your body. Also, weigh yourself daily and call your healthcare provider if you gain too much weight.
Key points
- Ascites is a condition in which fluid collects in spaces within your abdomen.
- As fluid collects in the abdomen, it can affect your lungs, kidneys, and other organs.
- Ascites causes abdominal pain, swelling, nausea, vomiting, and other difficulties.
- Stopping all alcohol intake, maintaining a healthy weight, exercising, not smoking, and limiting salt intake can help prevent cirrhosis or cancer that may lead to ascites.
- Ascites can’t be cured but lifestyle changes and treatments may decrease complications.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the names of new medicines, treatments, or tests, and any new instructions your provider gives you.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.